Therapy of glioblastomas
Therapy of glioblastomas
Motivation
Glioblastoma, also known as glioblastoma multiforme (GBM), is one of the most common and aggressive human brain tumors. This cancer is very difficult to treat. This is reflected in the success of therapy, as despite a multimodal approach consisting of surgery, chemotherapy and radiotherapy, the median survival time of GBM patients is usually less than 15 months. The 5-year survival rate of patients is also very low at about 10%. A defining feature of GBM is its high rate of infiltration into surrounding healthy tissue, resulting in a high risk of tumor recurrence. In most GBM patients, tumor recurrence occurs only a few months after treatment.
Aims and approach
Our aim is to further investigate the characteristic properties, such as invasiveness and migration of glioblastoma cell lines with respect to therapeutic treatment by irradiation and the application of chemotherapeutic agents, in order to better understand the effects of the particular therapy on tumor cell mobility. With this regard, it is important to identify the cellular mechanisms responsible for the development of therapy resistance. In this context, we are particularly interested in the role of cellular communication between individual cancer cells as a potential culprit for therapy resistance.
Innovations and perspectives
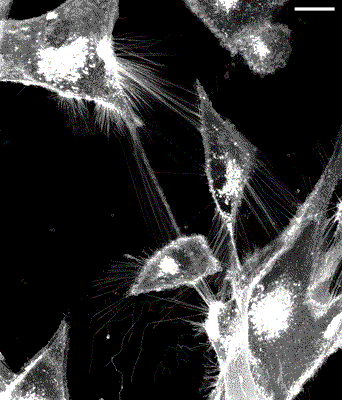
Our research is dedicated to so-called tunneling nanotubes (TNTs), which allow cells to communicate directly with each other. TNTs are membrane bridges between individual cells that enable a rapid and targeted exchange of information. It is particularly remarkable that cancer cells form large, extensive communication networks with the help of the TNTs and are thus able to communicate optimally with each other. These communication networks may potentially allow cancer cells to rapidly adapt their survival strategies and thus escape being killed by therapy.
With the help of our high-resolution Leica STED microscope, we are able to analyze in detail the development of TNT networks after treatment and further elucidate their role in cancer cell mobility.
If the TNT networks contribute to the aggressive behavior of glioblastoma cells, they could be used as a target for new therapeutic approaches, increasing the chances of successful treatment of glioblastoma.